7 Habits of Highly Efficient Physicians
Family physicians often spend 1.5 hours each night on EHR tasks, leading to burnout. These practical habits can help you reclaim your time while still delivering excellent care.


Popular articles
Research has shown that family physicians manage an immense administrative burden. One study found that family medicine doctors spend, on average, one and a half hours after work completing EHR tasks or paperwork. This nightly “pajama time” with the EHR leads to professional dissatisfaction and burnout. What habits do highly efficient physicians practice to leave their clinical notes at the office when they go home after a long workday?
Below are seven practical steps physicians can take to improve efficiency and reduce their time working after hours.
How do highly efficient physicians work?
Imagine what it would be like to close your office door at the end of the day and not have any work you need to take home. Incorporating these habits can help you reclaim your time while continuing to practice excellent care.
1. Pay attention to “how” and “why” as you start your day
Highly efficient physicians start their day with a clear purpose. It’s not just about how you manage your time but also about why.
For example, we all know how arriving at the office just in time for your first appointment can set your day off on the wrong foot. One habit of efficient physicians is to arrive early enough to check your schedule, answer messages, or huddle with your staff before your first visit. Arriving even 15 minutes earlier can set the day on a different course.
However, knowing why it's worth doing is key to building this habit. Think about a specific goal motivating you to get to the office early. You may have young children at home and want to get home early enough to eat dinner with them. Perhaps you’re a runner wanting to get outside before the sun goes down. Or maybe you’re motivated to improve your leadership at work, and you’ve found this extra time allows for a quick daily check-in with staff. If you pair specific habit changes with a clear articulation of your “why,” you’ll find it easier to stick with them.
2. Use previsit planning
Previsit planning can take many forms, but the goal is to consistently walk into each patient visit organized and ready. Highly efficient physicians will anticipate, during the current visit, what labs or X-rays will be needed at the next visit. Pre-ordering those tests a week before the next visit saves staff time contacting patients or searching for results during visits.
Another efficient habit is to have a medical assistant review the patient’s record on the day of the visit (or the day before) to see what prep work can be done based on the patient’s needs. Creating prep sheets for common conditions can also help.
3. Make every second count
Highly efficient physicians build the habit of squeezing small tasks into small amounts of time throughout the day. What do you do when you have five spare minutes while a team member preps the next exam room? Use that time to complete a prescription refill request, answer a message, or finish charting.
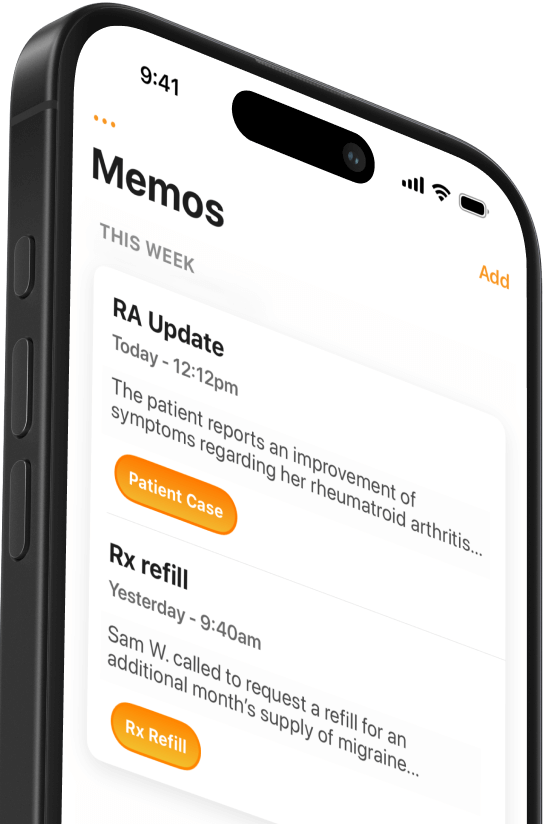
It’s much easier to build this habit if you have well-established workflows and the right technology. For example, many providers use mobile medical dictation apps like Mobius Conveyor to dictate clinical notes on their iPhones. You can even dictate a secure voice memo in the app and send it to your EMR when you’re back at the computer. Make sure you have the right medical practice software tools to make good use of downtime.
4. Rethink who does what
Being a highly efficient physician requires being a highly effective manager. Are there times throughout your workday when you wonder, “Why am I the one doing this task?”
If the answer is “yes,” this is an excellent opportunity to delegate the task to the most appropriate person. For example, have a medical assistant help with documentation, carry out needed screenings, or educate patients about a topic like inhaler use.
If your staff aren’t working at the top of their licenses, there might be ways you can empower them to do so. Their efficiency will affect yours, so supporting training and management opportunities is in your best interest.
5. Document less but better
Everyone has preferences about when and how they document. But it’s occasionally worth considering whether your preferences or processes might be hindering your documentation workflow.
The simple truth is that typing is the slowest way to complete clinical notes. Is it time to embrace the new technology–medical dictation, an AI scribe, or just EHR templates–to complete clinical notes faster? Many physicians are reticent to change their workflow and incorporate the latest time-saving solutions. If that sounds like you, here’s some inspiration from Dr. John Williams, M.D., F.A.C.S., a leading cancer surgeon and educator, talking about why he switched from typing to medical dictation:
“It’s easier to not change because of resistance, but it’s so worth the effort to flip that switch and integrate dictation because it’s something you’ll use forever going forward. I would bet there isn’t one doctor who has used a dictation system like Dragon or Mobius and then stopped using it and returned to typing text as the modality for communicating. There’s a reason no one returns to typing from dictation, and that’s because speaking is natural – it’s human.”
Over-documentation is another time-sucking habit that many physicians develop. It’s especially easy to get compulsive when you have to worry about medicolegal risk, are trying to gather rich psychosocial information, or feel pressured to check all the boxes you can. However, not all EHR boxes need checking, and most visits don’t require you to write an opus.
Occasionally, check in and ask whether you’re documenting more than necessary. Try setting a timer to measure your average time to complete a chart, or ask one of your most efficient colleagues what they do that helps speed up their documentation.
6. Touch messages once
Try to organize your clinical communication so messages go directly to the person who should handle them. Fewer handoffs are key to quality improvement, so you don’t want all messages funneled through you.
Similarly, you should check each of your messages only once. Read it, take action (respond or delegate), and move on to the next task.
When email and patient portals are always at our fingertips, combining the right technology with discipline is essential. Make sure the mobile apps you use for checking messages support all the functions you need and get in the habit of only checking messages when you have time to respond or manage them.
7. Help each other
If one physician in your practice consistently struggles to stay on top of their work, it’s up to the whole team to help them succeed. As a group of physicians write in FPM:
“If you see a physician struggling (or if this physician is you), the best approach involves empathy, mentoring, and accountability. The practice may need to set standards for when charts are expected to be closed – and enforce those standards. At the same time, a manager or colleague should work with the physician to figure out what's going on, what his or her barriers are, and how to get back on track. Maybe the physician needs to have some time blocked out on the schedule to catch up on charting. Maybe the physician needs some EHR training or an MA to help with in-room documentation. Or maybe the physician just needs some coaching because he or she is trying to do too much in the exam room (for example, trying to address everything on the patient's agenda, over-documenting, and not delegating tasks such as patient education).
The barriers and solutions are going to be personal because we are all programmed differently, but most physicians will need some help figuring things out. Don't let a colleague struggle alone, and don't make the mistake of simply applying more pressure on an already pressured physician.”
Remember, there's more to practice than efficiency
It’s important to remember that there's more to practice than efficiency. Efficiency can help you practice more effectively and avoid burnout, but be careful not to let it come at a cost.
We've gone too far if our desire to save seconds comes at the expense of quality care or supportive interactions with patients or staff. Just like building new habits, becoming more efficient requires ongoing check-ins to ensure that your clinical workflows align with your goals and values.
Related Articles

We Get Doctors Home on Time.
Contact us
We proudly offer enterprise-ready solutions for large clinical practices and hospitals.
Whether you’re looking for a universal dictation platform or want to improve the documentation efficiency of your workforce, we’re here to help.





